Facts About Maternal Suicide
Issue Brief: Maternal Suicide in the U.S.: Opportunities for Improved Data Collection and Health Care System Change
Click on an infographic to view larger and download the image to share on social media.
Recommended Citation:
Policy Center for Maternal Mental Health. (2023, September). Maternal Suicide in the U.S.: Opportunities for Improved Data Collection and Health Care System Change [Issue Brief]. https://www.2020mom.org/issue-briefs-and-papers
Maternal Suicide Awareness Month
Key Dates:
September
Suicide Awareness and Prevention Month and Maternal Suicide Awareness Month
The First Week of September
Maternal Suicide Awareness Week – Social media awareness activities are encouraged.
Partners can pull these facts about maternal suicide into their images and posts.
History of Maternal Suicide Awareness Week and Remembrance Vigil
The Policy Center for Maternal Mental Health (then 2020 Mom) launched the annual Maternal Suicide Awareness Week in 2018 during National Suicide Prevention Month to raise awareness about maternal suicide.
Then, research suggested suicide was a leading cause of maternal mortality; however, data on U.S. maternal suicide was not available. Our ultimate goal was to drive action in improving the reporting of maternal suicide rates in the U.S. and implementing programs to prevent maternal suicide.
During this time, we hosted webinars, provided fact sheets and social media toolkits and posts, and hosted the remembrance candlelight vigil with families impacted by maternal suicide to say the names of mothers lost.
Though the Policy Center no longer produces a social media toolkit annually, the Policy Center posts may be shared on social media, and/or facts can be pulled from our maternal suicide reference materials.
Past Maternal Suicide Social Media Awareness Campaigns:
• 2022 Campaign • 2021 Campaign • 2020 Campaign • 2019 Campaign
CDC Report on Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 US States, 2017–2019
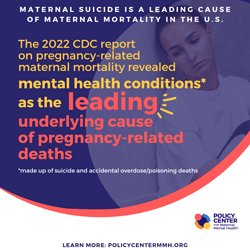
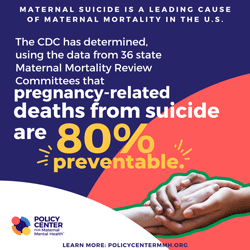
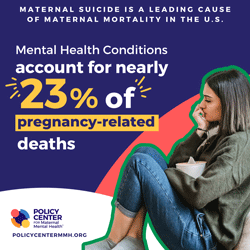
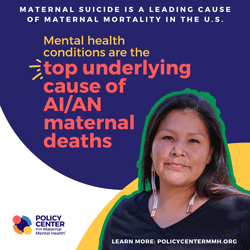
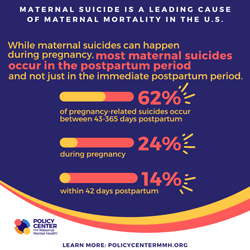
In September 2022, the CDC released a report on maternal mortality. Mental health conditions (including deaths by suicide and overdose/poisoning related to substance use disorder) were the leading underlying causes of pregnancy-related death, accounting for 23% of the deaths. More than 80% of pregnancy-related deaths were preventable. Read More →
The following are resources for those working to advance maternal suicide prevention and support.
U.S. Maternal Suicide Facts Sheet
Suicide is a preventable public health problem and a leading cause of death in the United States. More investment in suicide prevention, education and research will help prevent the untimely deaths of thousands of Americans each year.
Suicide Facts Sheet: United States Infographic
Click to download or print.
View citations here.
Past Maternal Suicide Webinars
The Latest in Maternal Suicide Trends Fireside Chat
Maternal Suicide in the U.S., The Latest Research & Data Collection Efforts 2022
Webinar link
Webinar slides
Executive Summary of the Upcoming Report on Maternal Suicide link
Blog: CDC: Maternal Mental Health Disorders are the Leading cause of Pregnancy-Related Deaths
Maternal suicide is a leading cause of maternal mortality. With efforts made by the policy organization, 2020 Mom, and the CDC, the U.S. has made significant progress on tracking and reporting maternal suicide rates. However the work to identify maternal suicides is left to the states through reviews conducted in Maternal Mortality Review Committee (MMRC) settings. Additionally, state-based Perinatal Quality Collaboratives (PQCs) are generally charged with facilitating change based on MMRC findings.
This webinar covers:
A general overview of maternal suicide statistics in the US
Updated data from the CDC on Maternal Mortality Review Committees and pregnancy-related suicide deaths.
How states are improving suicide detection in their MMRC process, including the role of informant interviews in identifying maternal suicide deaths, a process adopted by the Delaware MMRC and others
2020 Mom’s latest issue brief - suicide tracking and prevention
Colorado’s latest report illustrates suicide is the top cause of maternal death, and efforts the PQC is championing
Challenges and opportunities
Maternal Suicide in the U.S., The Latest Research & Data Collection Efforts
Thursday, September 30, 2021
Maternal suicide is a leading cause of maternal mortality. Despite common misconceptions, pregnancy and the postpartum period do not protect against the risk of psychiatric disorders or suicide. It has become increasingly urgent and important to normalize the discussion of maternal suicide to raise awareness and double-down on maternal suicide tracking and prevention efforts. In this webinar, we will cover:
A general overview of maternal suicide research and data collection in the U.S.
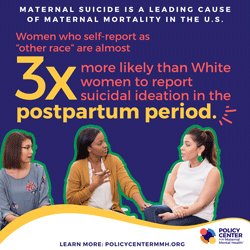
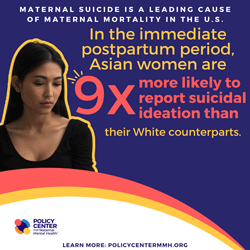
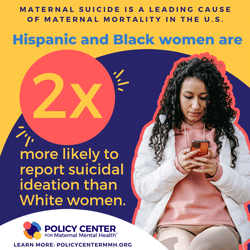
The difference between suicide risk and suicidal ideation, including racial disparities
Maternal suicide risk factors
Efforts to Standardize Review by Maternal Mortality Review Committees
PRESENTERS:
Sidra Goldman-Mellor, Ph.D., M.P.H.
Lead Investigator, Maternal drug-related death and suicide are leading causes of post-partum death in California
Associate Professor of Public Health
School of Social Sciences, Humanities, and Arts
Director, HSRI Biostatistics and Data Support
University of California, Merced
Marcela Smid, MD MA MS
Lead Investigator: Pregnancy-Associated Death in Utah: Contribution of Drug-Induced Deaths
Assistant Professor, Division of Maternal Fetal Medicine
Department of Obstetrics and Gynecology
University of Utah
Medical Director of SUPeRAD (Substance Use and Pregnancy - Recovery, Addiction, Dependence) Clinic
Kara Zivin, PhD, MS, MA, MFA
Researcher and Peer with Lived Maternal Mental Health Experience
Lead Investigator, Trends in Suicidal Ideation and Self-Harm Among Privately Insured Delivering Women
Professor of Psychiatry, Obstetrics and Gynecology, Health Management and Policy/Public Health
University of Michigan
Faculty Associate, Survey Research Center
Institute for Social Research
Research Career Scientist, Center for Clinical Management Research (CCMR),
VA Ann Arbor Healthcare System
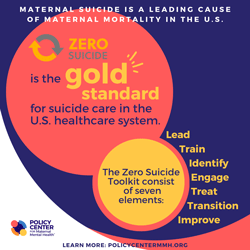
2020 Mom and our partner, Zero Suicide Institute, learned and discussed the national Zero Suicide framework, a system-wide, organizational commitment to safer suicide care in health and behavioral health care systems.
The framework is based on the realization that suicidal individuals often fall through the cracks in a sometimes fragmented and distracted health care system. A systematic approach to quality improvement in these settings is both available and necessary.
Inspired by health care systems that had seen dramatic reductions in patient suicide, the Zero Suicide began as a key concept of the 2012 National Strategy for Suicide Prevention and quickly became a priority of the National Action Alliance for Suicide Prevention (Action Alliance), and a project of Education Development Center's Suicide Prevention Resource Center (SPRC), supported by the Substance Abuse and Mental Health Services Administration (SAMHSA).
The U.S. health delivery system was already struggling to effectively address and prevent suicide, now with pandemic stressors expected to increase suicide rates, health systems can take action by adopting the Zero Suicide framework and tools.
Moderator:
Joy Burkhard, MBA
Executive Director, 2020 Mom
Panelists:
Julie Goldstein
Director, Zero Suicide Institute
Edwin Boudreaux, PhD
Professor, Departments of Emergency Medicine, Psychiatry, and Population and Quantitative Health Sciences
University of Massachusetts Medical School
Maternal Suicide: What All Providers and Advocates Should Know
(Click title to view.)
September 29, 2020
Hosted by:
Presenters:
SUSANNA TROST, MPH
Maternal Suicide Stats
CDC Maternal Mortality Prevention Team, Division of Reproductive Health
JENNIFER BEAUREGARD, PhD
CDC Maternal Mortality Prevention Team, Division of Reproductive Health
MARY CLAIRE KIMMEL, MD
Maternal Mental Health
Suicide Nuances
Assistant Professor, Department of Psychiatry at University of North Carolina at Chapel Hill
KAREN TABB DINA, PhD
Differences in Maternal Suicidal
Thoughts in BIPOC Community
University of Illinois at Urbana-Champaign
RACHAEL KENTER, MPH, CHES
Upstream Prevention
& Zero Suicide Initiative
Suicide Prevention Resource Center
SHYE LOUIS, M.Ed.
Crisis Prevention
National Suicide Prevention Lifeline
In this webinar, we covered the latest on suicide prevention and facts about maternal suicide, including:
A general overview of suicide and COVID related increases
Maternal mental health statistics including maternal suicide
General crisis prevention efforts
Suicide prevention efforts
View presentation slides here.
Suicide Prevention Resources
The American Foundation for Suicide Prevention has resources to assist with setting and communicating policy priorities on suicide prevention, as well as infographics to share.
Read about CDC’s suicide prevention strategic plan, grounded in data, science, action, and collaboration.
Explore CDC’s Preventing Suicide: A Technical Package of Policies, Programs, and Practices for strategies and approaches with the best available evidence to prevent suicide.
The Zero Suicide Toolkit: a detailed guide to Zero Suicide implementation and strategy.
The Collaborative Assessment and Management of Suicidality (CAMS): a flexible therapeutic framework in which patient and provider work together to assess the patient’s suicidal risk and use that information to plan and manage suicide-specific, “driver-oriented” treatment. It is a philosophy of clinical care that can be used for a wide range of suicidal patients across outpatient and inpatient treatment settings and in the context of various psychotherapies and treatment modalities.
Care Transitions Outpatient Health Care Self-Assessment from National Action Alliance for Suicide Prevention
The Outpatient Self-Assessment is a checklist designed to help outpatient behavioral health care systems assess their policies, procedures, and practices as they compare to the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care. The results of the self-assessment will help outpatient health care systems identify opportunities to improve administrative practices and clinical care.
Outpatient Care Transitions Action Planning template from National Action Alliance for Suicide Prevention. The Outpatient Action Planning template was developed to translate the results of the self-assessment into action steps that will incrementally improve their overall care transitions and patient care practices.
Suicide Safety Plan: A safety plan app that allows you to customize your own warning signs that a crisis may be developing, coping strategies for dealing with suicidal urges, places for distraction, friends and family members you can reach out to, professionals you can call, methods of making your environment safe, and your own important reasons for living.
Guide on Suicide and Serious Mental Illness
Click to view the 5 page pdf.
People who live with serious mental illness (SMI)—such as major depression, bipolar disorder, and schizophrenia—are at increased risk of suicide. It is critical to understand the problem of suicide for those who have SMI. That is the only way to create a comprehensive, effective suicide prevention plan.
SMI Adviser and the Suicide Prevention Resource Center (SPRC) are proud to present a new guide on Suicide and Serious Mental Illness. It is an ideal resource for both suicide prevention coordinators and mental health clinicians.
Why Screen for Maternal Suicide Risk?
Screening for maternal suicide risk is critical in both saving lives and also in preventing unintentional harm to mothers and families. Given the frequency of unwanted “intrusive thoughts” during the perinatal period, which can involve thoughts of self-harm, it’s critical that providers screen for both ideation and risk.
Screening Tools
Several suicide screening tools exist; the Columbia Suicide Severity Rating Scale (C-SSRS) is robust in assessing for ideation and risk.
The Columbia-Suicide Severity Rating Scale (C-SSRS) is a tool that can be used in many settings, including, community settings, medical, inpatient, and outpatient behavioral health.
The C-SSRS assesses the full range of evidence-based ideation and behavior. It can be used as an initial screener or as part of a full assessment.
Those who administer the screening for maternal mental health disorders may wish to use the C-SSRS if a person verbally discloses suicidal thoughts or answers “yes” to question 9 on the PHQ-9 or question 10 on the EPDS, for example.
Additionally, the SAFE-T Suicide Assessment Five-Step Evaluation and Triage may be utilized to understand both access to potential deadly tools and protective factors.
Download the C-SSRS or combined C-SSRS & SAFE-T tools here:
Or you can create your own screening toolbox by visiting the Columbia C-SSRS Lighthouse Project’s website.
Free Training
Though training is not required to administer the screener, it can be helpful. Training provides an overview of the C-SSRS instrument and teaches how and when to administer it in real-world settings
Watch a Pre-Recorded Webinar
Watch a webinar on your own schedule by going to the Columbia University C-SSRS Light House Project’s YouTube channel and selecting an archived webinar. They are available in 30 languages and are less than an hour long.
Safety Plan Template
A safety plan is designed to guide you through a crisis. As you proceed through the steps, you can help yourself and feel safer. Keep your plan easily accessible in case you have thoughts of hurting yourself.
Click to view the 2 page pdf.
Monitoring Federal and State Maternal Suicide Reporting Efforts
The blog posts below share our analyses of how the U.S. is progressing in its journey to report a national maternal suicide rate. Follow our blog by signing up for 2020 Mom's enews to keep abreast of the slow but steady efforts and progress being made.
Maternal Suicide: The US Should Measure What It Treasures
U.S. Has the Highest Suicide and Maternal Mortality Rates Among Wealthy Nations
Maternal Suicide Tracking in the U.S. – We’re Getting Closer
The Latest Data on Maternal Mortality (Including Suicide) in the US & CA